A recent survey of 100 healthcare leaders within finance, revenue cycle, reimbursement, and health information 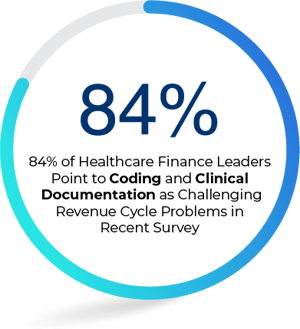 management at hospitals and acute-care facilities sought to report on the areas of most-needed improvement within revenue cycle management. The results of the survey, by BESLER who partnered with HIMSS, found a significant majority of respondents -- 84% noted coding and clinical documentation as two areas of high or medium revenue cycle risk. Nearly half noted these two areas as their greatest vulnerability. Why are these two areas causing such concern among leaders and resulting in depleted revenues?
management at hospitals and acute-care facilities sought to report on the areas of most-needed improvement within revenue cycle management. The results of the survey, by BESLER who partnered with HIMSS, found a significant majority of respondents -- 84% noted coding and clinical documentation as two areas of high or medium revenue cycle risk. Nearly half noted these two areas as their greatest vulnerability. Why are these two areas causing such concern among leaders and resulting in depleted revenues?
A core reason cited for the problems with coding and clinical documentation are they are not properly setup for diagnosis-related group (DRG) payments. For some context, DRG is how Medicare and some insurance firms can build categories for hospital costs in order to calculate patient’s payment obligations. It’s intended to prevent overtreatment issues and add efficiency to hospital care. Nearly 70 percent of respondents said their solutions cannot manage DRG coding, a significant issues since it is used by Medicare and other major payers.
The vulnerabilities found in coding and clinical documentation arise mainly because DRG payments systems are constantly evolving. This dynamic environment means hospitals have to keep track of frequent changes which makes it much harder to produce accurate coding. Low-quality coding means carrier denials and inaccurate reimbursements—two problems noted by nearly 50 percent of the survey respondents. Despite the pressing need for improvements of DRG coding and documentation, providers are oftentimes restricted by factors including budget constraints, unclear ROI, lack of qualified staff, and entrenched current solutions.
Hospitals and acute-care facilities can reduce coding and documentation vulnerabilities by working with Aviacode, a leading provider of medical coding and compliance services. The company earned designation from Modern Healthcare last year as one of top-ten largest revenue cycle management firm in the country.
Aviacode’s 700+ experienced and credentialed coders accurately code more than 10 million encounters per year for a variety of clients. This high-quality team knows how to reduce coding errors and help identify ways to significantly improve documentation—turning vulnerabilities into opportunities.


