Coding audits provide insight into the process of coding itself according to ICD10Monitor's article entitled "Coding Audits: A Compliance Necessity". Although coding audits typically include the review and analysis of the medical record documentation and coding, the article also suggests that one should also review coding policies and procedures, as well as coding operational functions.
Read More
Topics:
ICD-10,
Clinical Documentation,
Medical Coding Audits,
Outsourcing,
CDI
The U.S. Department of Health and Human Services Office of the Inspector General (OIG) recommended earlier this month that the U.S. Centers for Medicare & Medicaid Services (CMS) should recoup the portion of nearly $1 billion that was incorrectly paid to hospitals because of medical coding and billing errors involving severe malnutrition diagnosis codes in FYs 2016 and 2017.
Read More
Topics:
ICD-10,
Medical Coding,
Clinical Documentation,
Medical Coding Audits,
Pro-Fee Coding,
Facility Coding,
Outpatient Coding
Coding audits, which are the validation of code assignment against the supporting clinical documentation and coding guidelines, are an instrumental way to ensure accuracy. Organizations usually conduct regular coding audits as directed by their internal compliance plan. They include a random sampling of records or encounters reviewed per coder during a specified timeframe, typically on an annual basis.
Read More
Topics:
Clinical Documentation,
Medical Coding Audits
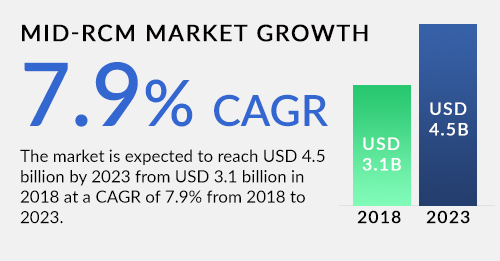
Mid-revenue cycle management is concerned with the phase of the process between the point where a patient accesses care and the care provider’s business office. Typically processes during this time include documentation, coding, CDI, and compliance. A recent Markets and Markets report expected sustained growth in this market. It projects a compound annual growth rate (CAGR) of 7.9 percent and a market size of $4.5 billion by 2023.
Read More
Topics:
Revenue Cycle Management,
Medical Coding,
Clinical Documentation,
CDI
By optimizing revenue healthcare, organizations can put themselves in a position to survive and thrive in the modern marketplace of shrinking margins, consumer engagement, and higher cost pressures. This is true whether you are affiliated with billing companies, hospitals, physician practices, or payers. One of the most important ways to optimize revenue is by ensuring accuracy and efficiency in medical coding and documentation.
Read More
Topics:
Medical Coding,
Clinical Documentation,
HCC Coding,
Medical Coding Audits
Coordinated Health and its founder and CEO entered recently into an agreement with the federal government to settle False Claims Act allegations, according to the Department of Justice. The health system will pay $11.25 million and founder and CEO Emil Dilorio, MD will pay $1.25 million to settle the allegations. In addition to the monetary settlement, the system entered into a corporate integrity agreement with HHS that will require monitoring of its billing practices for five years.
Read More
Topics:
Clinical Documentation,
Coding Compliance,
Outsourcing
A recent Becker’ Hospital CFO Report article noted the changing of the rules governing reporting of social determinants of health following the American Hospital Association's diligent work. The association said the ICD-10-CM Cooperating Parties, including AHIMA, AHA, CMS and the National Center for Health Statistics, approved advice published by the AHA Coding Clinic that allows hospitals to report ICD-10-CM codes included in categories Z55-Z65, based on documentation from all involved caregivers, including non-physicians. That change took effect in February of this year.
Read More
Topics:
Medical Coding,
Clinical Documentation,
Outsourcing
The Centers for Disease Control and Prevention (CDC) released the fiscal year (FY) 2019 ICD-10-CM (diagnosis) code changes last month. There are 473 code changes beginning October 1, 2018. They include 279 new codes, 143 revised codes, and 51 deactivated codes, according to the CDC website. In addition, there were 39 additional changes added from the proposed rule (list). The ability to code properly to these new and revised codes starting October 1 can make the difference in getting clean claim and being paid quickly or needless reimbursement delays.
Read More
Topics:
Medical Coding,
Clinical Documentation,
Outsourcing
Clinical documentation improvement (CDI) ensures that health services are accurately documented and helps healthcare coders and physicians work toward improved patient care, while also streamlining productivity. When meaningful clinical data is captured, organizations can ensure improved quality reporting, clinician productivity, and even better – accurate clinical information is delivered at the point of care.
Read More
Topics:
Medical Coding,
Clinical Documentation,
Outsourcing
A recent study reported in a Los Angeles Times article found that healthcare in the United States is very expensive. One of the contributing reasons is that managing healthcare bills is really expensive. How expensive? At one large academic medical center, the cost of collecting payments for a single primary care doctor is upward of $99,000 a year.
Read More
Topics:
Medical Coding,
Clinical Documentation,
Outsourcing,
Coding Denial Management