2020 presented daunting challenges to the healthcare industry, not only in diagnosing and treating COVID-19 patients, but also in transforming a healthcare delivery system to modern needs. There were hyper-growth adoptions in telehealth as more providers and the public embraced technology for patient engagement. Remote workforce, which has been common for companies like Aviacode for years, became the norm for many, who had to learn new processes if they hadn't been doing remote work before. This was true for medical coders and healthcare RCM workers alike.
Read More
Topics:
Revenue Cycle Management,
Medical Coding,
Medical Coding Audits,
Outsourcing,
COVID-19
A recent Becker's Hospital Review article highlighted healthcare's significance in the American economy. In that, healthcare accounts for more than 17 percent of the nation's gross domestic product, employs more people than any other industry in the nation, and venture capital alone invested more than $23 billion in healthcare in 2018. The article points out that despite these massive investment and the efforts of a talented workforce, many of the nation's hospitals and health systems operate on razor-thin operating margins and face the dual challenge of achieving fiscal sustainability while delivering high quality care to patients.
Read More
Topics:
ICD-10,
Revenue Cycle Management,
Medical Coding,
Pro-Fee Coding,
Facility Coding
Major medical groups and hospitals have backed the CMS' decision to abandon a provision of the finalized 2019 Medicare Physician Fee Schedule rule that would have consolidated the number of Evaluation and Management (E/M) payment levels into one payment rate beginning in 2021. The agency initially proposed the E/M coding measure in the belief that it would reduce clinicians' work to get Medicare reimbursement. However, providers worried that lower reimbursement rates would cut into their bottom lines and create a number of unintended consequences that could hurt patients.
Read More
Topics:
Revenue Cycle Management,
Medical Coding
Managers of skilled nursing facilities are eagerly anticipating changes that will change the way they code, bill, collect data, and operate. A September 2019 article from McKnight’s Long-Term Care News details the long-awaited changes for long-term care reimbursements through the new Patient-Driven Payment Model (PDPM). The changes, which go into effect October 1, are revisions to the Resident Assessment Instrument (RAI), which is essentially the “rulebook” for Medicare and Medicaid reimbursements.
Read More
Topics:
Revenue Cycle Management,
Medical Coding
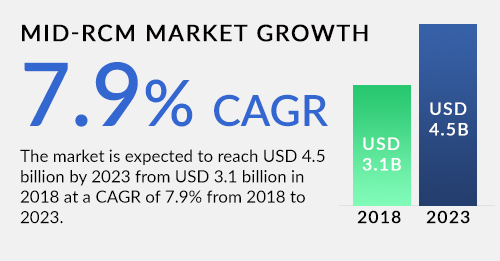
Mid-revenue cycle management is concerned with the phase of the process between the point where a patient accesses care and the care provider’s business office. Typically processes during this time include documentation, coding, CDI, and compliance. A recent Markets and Markets report expected sustained growth in this market. It projects a compound annual growth rate (CAGR) of 7.9 percent and a market size of $4.5 billion by 2023.
Read More
Topics:
Revenue Cycle Management,
Medical Coding,
Clinical Documentation,
CDI
Aviacode joins AHIMA in celebrating and showing our appreciation for all the outpatient coding professionals during the month of September.
Read More
Topics:
Revenue Cycle Management,
Medical Coding
A recent Managed Healthcare Executive magazine article entitled: “Five ways to reduce healthcare administrative costs,” identifies five strategies that healthcare executives can use to reduce onerous administrative costs. According to the article, administrative costs make up about 15 percent of all healthcare expenditures -- well over $300 billion annually, as found in the 2016 index report from the California Association for Healthcare Quality. Outdated, manual processes and rejected claims eat up a large portion of this administrative cost.
Read More
Topics:
Revenue Cycle Management,
Medical Coding,
outsource
Medicare Advantage (MA) is a complex program that continues to gain popularity, with about one-third of Medicare beneficiaries currently enrolled in a variety of MA programs. MA plans are issued by MAOs, or Medicare Advantage Organizations, that are typically insurance companies.
Read More
Topics:
Revenue Cycle Management,
Medical Coding,
HCC Coding
Not only is clinical documentation improvement (CDI) the key to better ICD-10 coding and reimbursement accuracy, but it's also vital for preparing healthcare organizations for the new care paradigm of population health management. To this end, AHIMA has designated the month of July as CDI Month with Aviacode joining in the recognition to CDI professionals nationwide.
Read More
Topics:
Revenue Cycle Management,
Medical Coding,
Clinical Documentation

There are two key players in revenue cycle stream – the HIM coding department and the patient financial services department. Working together these two departments can sustain a healthy revenue cycle for any healthcare organization. These two departments are responsible for all of the basic elements of the revenue cycle -- from registration to coding the care provided to final discharge.
Patient financial services, typically, includes the registration process, and that is where the revenue stream has its head waters. An accurate registration process establishes the basis for future follow-up with payers or the patient as a self-payer.
Using their knowledge of billing rules, patient financial services applies the appropriate billing rules, such as Local Medical Review Policies (LMRPs) or National Coverage Determinations (NCDs) to produce an accurate patient bill.
The HIM coding department uses its vast knowledge of the very latest coding rules to provide patient financial services with an accurate medical record from which to produce their patient bill.
Read More
Topics:
Revenue Cycle Management,
Medical Coding,
Denial Management